In June 2025, the World Health Organization (WHO) released its first global guideline on managing of sickle cell disease (SCD) during pregnancy, marking a significant step in improving maternal and neonatal health outcomes. The guideline highlights the increased risks faced by pregnant women with SCD, who are more vulnerable to complications such as preeclampsia, preterm birth, and maternal mortality. With over 20 evidence-based recommendations, WHO aims to standardize and enhance care across both high- and low-resource settings. This initiative emphasizes the urgent need to expand access to safe, respectful, and informed healthcare for affected women worldwide.
Understanding Sickle Cell Disease: Scope, Burden, and Prevalence
Sickle cell disease (SCD) is a hereditary blood disorder caused by the production of abnormal hemoglobin, known as hemoglobin S. This leads to the formation of crescent-shaped red blood cells that are less flexible and can obstruct blood flow, resulting in severe pain, anemia, infections, and progressive organ damage.
The rising prevalence of SCD reflects a significant global health concern. According to the World Health Organization (WHO), approximately 7.7 million individuals are living with SCD worldwide, with over 375,000 deaths reported annu ally. The condition is most common in malaria-endemic regions, particularly sub-Saharan Africa, which accounts for nearly 80% of global cases. In the United States, the Centers for Disease Control and Prevention (CDC) reports that about 100,000 people are affected, predominantly among non-Hispanic Black or African American populations.
Pregnancy and Sickle Cell Disease: A High-Risk Intersection
Pregnancy in women with SCD carries a significantly higher risk of complications. These include preeclampsia, blood clots, preterm labor, and maternal and neonatal mortality. According to the CDC Foundation, individuals who live with SCD are more vulnerable to these life-threatening complications compared to those without the condition. A research study by Mimi Yue et al. (2024) indicates that approximately 300,000 babies are born with SCD each year, mostly in low- to middle-income regions. In countries such as Australia, migration trends and longer life expectancy are contributing to a rise in pregnant women with SCD, necessitating improved, multidisciplinary prenatal care systems to manage this emerging healthcare challenge.
WHO Guidelines on Managing Sickle Cell Disease in Pregnancy: Purpose, Scope, and Development Approach
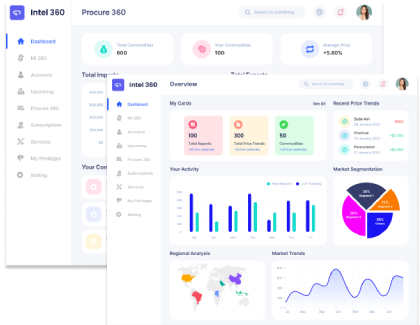
The World Health Organization (WHO) has recently published guidelines to address the management of sickle cell disease (SCD) during pregnancy, childbirth, and the postnatal period. This initiative was informed by a structured scoping process undertaken in 2021 to identify priority areas within noncommunicable diseases affecting maternal health. The primary objective of the guideline is to provide evidence-based recommendations that promote consistent clinical decision-making and improved maternal and perinatal outcomes across healthcare systems globally.
The scope of the guideline encompasses key aspects of clinical care, including medication use, pain and fluid management, thromboprophylaxis, fetal surveillance, timing of delivery, and interpregnancy care. Recommendations were formulated using the PICO (Population, Intervention, Comparator, Outcome) framework to address prioritized clinical questions. The target audience includes healthcare providers, policymakers, and program managers operating within varied resource settings.
The guideline was developed following WHO’s standardized process for guideline development, as outlined in the WHO Handbook for Guideline Development. This involved six main steps: defining key questions, retrieving and appraising evidence, synthesizing findings, formulating recommendations, and planning for dissemination and future updates. A multidisciplinary Guideline Development Group (GDG) and Evidence Synthesis Group (ESG), supported by methodological experts, applied tools such as GRADE and GRADE-CERQual. In addition, expert consensus was incorporated to ensure clinical relevance, methodological rigor, and global applicability, wherever direct evidence was limited.
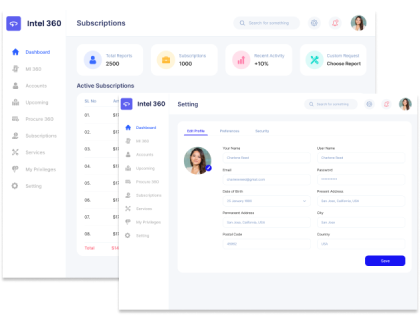
WHO Clinical Recommendations: A Framework for Safe and Effective Pregnancy Management in Sickle Cell Disease (SCD)
The World Health Organization (WHO) has established a structured set of clinical recommendations to guide safe maternal and fetal outcomes in pregnancies complicated by sickle cell disease (SCD). These are based on a comprehensive review of physiological data, WHO's existing clinical frameworks, and expert consensus in areas lacking strong empirical evidence. The following table presents key guidance areas, including medication safety, transfusion protocols, thromboprophylaxis, infection prevention, and delivery planning, tailored to the unique clinical needs of pregnant women with SCD. Each recommendation is designed to be adaptable based on resource availability, patient condition, and health system capacity.
| Clinical Area |
WHO Recommendation |
Supporting Evidence/Considerations |
| Folic Acid & Iron Supplementation |
5 mg folic acid daily (unless on sulfadoxine-pyrimethamine: 400 µg); iron only if deficiency is confirmed |
Prevents neural tube defects, risk of iron overload from transfusions, uses ferritin (adjusted for inflammation) to assess iron status |
| Prophylactic Blood Transfusion |
Consider women with recurrent crises or past benefits |
Reduces crisis frequency (RR 0.28); assesses alloimmunization and iron overload; has limited feasibility in low-resource settings |
| Hydroxycarbamide Use |
May continue or reintroduce after the 1st trimester in severe cases through shared decision-making |
Effective in non-pregnant populations; limited human data suggest no increased teratogenic risk |
| Anticoagulation/Thromboprophylaxis |
LMWH (low molecular weight heparin) preferred; UFH (unfractionated heparin) as an alternative in renal impairment or resource-limited settings |
SCD and pregnancy increase thromboembolism risk; evaluate other VTE risk factors; plan timing around delivery |
| Infection Screening |
Routine prophylactic antibiotics not advised; frequent screening (esp. UTIs) recommended |
Higher infection risk in SCD; antimicrobial resistance concerns; focus on early detection and targeted treatment |
| Pain Management |
Use paracetamol; use NSAIDs with caution (avoid 1st & 3rd trimesters); opioids at lowest effective dose |
Multidisciplinary pain plans should be initiated early, and ensure individualized, safe, and effective pain control |
| IV Fluid Management |
Monitor closely for overload and pulmonary edema; use isotonic crystalloids |
Evidence from non-pregnant SCD populations suggests risk of adverse outcomes; adjust for pregnancy physiology |
| Fetal Monitoring |
Ultrasound every 4 weeks from 24-32 weeks, every 3 weeks thereafter; more frequent if complications arise |
Addresses risks of growth restriction, placental pathology, and stillbirth; use of Doppler and biometry helps guide timely intervention |
| Birth Timing & Mode |
Early-term birth (37–38 weeks) may be considered in select cases; vaginal delivery preferred unless contraindicated |
Balance between continuation risks and fetal maturity; no routine caesarean without medical indication; clinical judgment and shared decision-making are key |
| Interpregnancy and Postnatal Care |
Integrated care with thromboprophylaxis, breastfeeding guidance, contraception, and newborn screening |
Hydroxycarbamide may be used during lactation if benefits outweigh risks; progestogen-only contraceptives are considered safe; multidisciplinary follow-up is strongly advised |
Global Implications and Strategic Future Course
The global dissemination and implementation of the WHO guidelines represent a critical step toward improving maternal and perinatal health outcomes, particularly in settings with a high burden of sickle cell disease in pregnancy. Effective integration into national policies requires structured collaboration among international agencies, ministries of health, and professional associations. Translating the recommendations into locally adapted care packages, supported by evidence-based tools, training programs, and monitoring frameworks, will facilitate sustainable implementation. Future directions should prioritize capacity building, equitable resource distribution, and context-specific adaptation to ensure long-term impact and health system resilience.
WHO’s guideline on managing sickle cell disease in pregnancy represents a significant advancement in global maternal health. By offering structured, evidence-based recommendations, it provides a unified framework to address the complex risks associated with SCD during pregnancy. Its successful implementation, particularly in resource-limited settings, depends on coordinated efforts across health systems. Strengthening provider capacity and promoting equitable access to care are essential to improving outcomes for mothers and newborns worldwide.















Share