Healthcare Workforce Challenges in Malaysia Impacting Hospital Efficiency and Patient Care
As Malaysia's healthcare system grows, one of its greatest challenges is to sustain an adequate and skilled healthcare workforce. Demand for medical practitioners is also growing very quickly due to increasing population, aging populations, prevalence of non-communicable diseases, and growth in hospital infrastructure. Supply, though, is lagging.
Public and private hospitals nationwide are facing deficiencies of doctors, nurses, and allied health professionals. These human resource limitations impact the delivery of services, enhance staff burnout, and undermine patient experience. Unless addressed, such issues can constrain Malaysia's healthcare sector long-term growth and capacity to treat domestic and foreign patients.
At the same time, hospitals are trying to hold on to their staff by making their working conditions better offering them chances to advance in their careers and helping them with their mental health. The government is also teaming up with companies to offer scholarships and other incentives to lure healthcare workers to rural areas where they are really needed.
Critical Shortage of Nurses and Specialists
A major shortfall in Malaysia’s healthcare workforce is the lack of qualified nurses and doctors in specialist areas. Reports across the board cite Malaysia as having fewer nurses per capita than the world average. This is particularly crucial in public hospitals where caregivers can exceed the patient ratio recommended by standard practice.
Also, there is a shortage of specialties, such as anesthesiology, cardiology, oncology and radiology. This is also more prevalent in the more remote/rural areas following the lack of retention incentives. Due to the workforce, hospitals in urban areas are at capacity, while rural hospitals are doing the exact opposite.
Hospitals are focusing on retention programs, better pay and international recruitment to replenish the shortfalls.
Urban-Rural Imbalance and Brain Drain
One issue faced in Malaysia's healthcare talent pool is the equity relating to urban-rural distribution of professionals. Most professionals prefer working in urban areas such as Kuala Lumpur, Penang, and Johor Bahru as these facilities are better equipped, which also offer better career growth prospects.
On the other hand, the lack of housing options, infrastructure, and access to ongoing medical education in rural hospitals in Sabah, Sarawak, and other remote locations deters doctors from relocating there.
Furthermore, brain drain is an issue. Many Malaysian physicians and nurses seek better-paying jobs or better working circumstances abroad, particularly in Singapore, Australia, and the United Kingdom. The local system is under more strain because of this talent migration.
Education and Training Gaps
Malaysia needs simpler, large-scale models for enhancing their healthcare talent pipeline, but must first develop a more effective pipeline of qualified health professionals. They still have gaps in both medical and nursing education, some institutions do not have new curricula to address recent advances in clinical technologies and patient care. There are also long and poorly supported transitions postgraduate education and work, particularly junior doctors in the obligatory internship.
Some allied health professionals still experience rigid route maps of training: medical technologists and physiotherapy providers still experience similar challenges and ongoing reach in workflow & layer on to hospital congest claims to see patients. Moving forward, increased medical education volume, levels of training and educational pathways and to improve systems and opt to elongate recommended routes to health worker, have longer term impacts on the systematic bottleneck of too many health professional seekers working inefficiently.
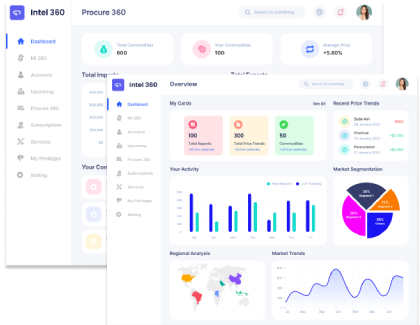
Technological Integration and Automation
As a result of the workforce shortage, many, if not, all hospitals in Malaysia are embracing 'embolden or assess' digital health or transporting to the simply advanced dimensions of healthcare service organization. Of course, EMR, AI or patient-supported diagnostic review and even remote patient monitoring results in deliverables that divide time away from a practitioner’s clinical administration load and provide them with opportunities to allocate more sustainable resources towards patient care-related functions.
Hospital operational functions or unit like billing by robotic process automations (RPA), or even pharmacy automation will enable hospitals to be operationally viable if staffing alone is difficult. The funding, digital literacy and societal normative valued behaviors will continually limit broader approaches and undermine technology as leverage.
For a comprehensive analysis and future forecast, read our Malaysia Hospital Market
Strengthening Malaysia’s Healthcare Workforce for the Future
The workforce issues in Malaysia's hospitals are complex, interrelated challenges, encompassing shortages and skill gaps, education, and retention issues that must be tackled collectively by the government, educational institutions, and health care providers. Investing in the human capital, fair distribution of talent across hospitals, and use of digital solutions will enable Malaysia to build a more robust and sustainable health workforce. Addressing these pressing challenges will ensure that hospitals in Malaysia consistently supply quality care and meet the demands of their growing and ageing populations.
















Share